Medical Policy
Policy Id
Topic
Section
Effective Date
Issued Date
Last Revision Date
Annual Review
Prepared By
DISCLAIMER
Highmark medical policy is intended to serve only as a general reference resource regarding coverage for the services described. This policy does not constitute medical advice and is not intended to govern or otherwise influence medical decisions.
POLICY STATEMENT
This policy provides information regarding the coverage of, as determined by applicable federal and/or state legislation.
This policy is designed to address medical necessity guidelines that are appropriate for the majority of individuals with a particular disease, illness or condition. Each person’s unique clinical circumstances warrant individual consideration, based upon review of applicable medical records.
The qualifications of the policy will meet the standards of the National Committee for Quality Assurance (NCQA) and the Delaware Department of Health and Social Services (DHSS) and all applicable state and federal regulations.
Purpose
This medical policy outlines Highmark Health Options services for Abdominoplasty and Panniculectomy.
Definitions
Highmark Health Options (HHO) – Managed care organization serving vulnerable populations that have complex needs and qualify for Medicaid. Highmark Health Options members include individuals and families with low income, expecting mothers, children, and people with disabilities. Members pay nothing to very little for their health coverage. Highmark Health Options currently services Delaware Medicaid: Diamond State Health Plan (DSHP), Delaware Healthy Children Program (DHCP), and Diamond State Health Plan Plus (DSHP) LTSS members.
Abdominoplasty – Abdominoplasty is typically performed for cosmetic purposes, involves the removal of excess skin and fat from the pubis to the umbilicus or above, and may include tightening of the rectus muscle and creation or transposition of the umbilicus.
Panniculectomy – A surgical procedure used to remove a panniculus, which is an apron of fat and skin that hangs from the front of the abdomen. In certain circumstances, the panniculus can be associated with skin irritation and infection due to interference with proper hygiene and constant skin-on-skin contact in the folds underneath the panniculus. The presence of a panniculus may also interfere with daily activities.
Computed tomography – Computed tomography, also referred to as “CAT scanning,” provides a different form of imaging known as cross-sectional imaging.
Panniculus – The subcutaneous fat or a layer of fat underlying the dermis (also referred to as pannus, fat apron, or abdominal apron). The layer of fat and dermis hangs from the front of the abdomen.
Lipectomy – The excision of subcutaneous adipose tissue which may be performed on various parts of the body (also referred to as belt lipectomy, liposuction, brachioplasty, buttock or thigh lift, and body lift).
Massive Weight Loss (MWL) – Loss of 50% of excess weight.
Functional Impairment – A condition that describes a state where an individual is physically limited in the performance of activities of daily living (ADL).
Intertrigo – An inflammation of the top layers of skin caused by moisture, bacteria, or fungi in the folds of the skin.
Colostomy – The surgical creation of an opening in the abdominal wall (belly). The end of the colon is brought through this opening to form a stoma. Colostomies are performed for many different diseases and problems.
Ventral hernia – A bulge or tear in the abdominal wall, resulting from weakened fascia or muscles, which allows the inner lining of the abdomen and/or intestinal loop to extend through the abdominal wall.
Incisional hernia – The most common ventral hernia. If the ventral hernia occurs along an area of a previous surgical incision, it is referred to as an incisional hernia.
“True” hernia repair – Involves opening fascia and/or dissection of a hernia sac with return of intraperitoneal contents back to the peritoneal cavity. A “true” hernia repair should not be confused with diastasis recti repair, which is the repair to the separation of the rectus abdominis muscles.
Policy Position
Prior Authorization
Prior Authorization may be required. Please validate codes on the Prior Authorization Lookup Tool https://www.highmarkhealthoptions.com/providers/prior-auth-lookup
Procedures
Abdominoplasty and panniculectomy following massive weight loss are clinically proven and, therefore, medically necessary procedures when all of the following criteria are met (American Society of Plastic Surgeons, 2017; Mechanick, 2013):
- A board-certified plastic surgeon performs the surgical procedure to modify the skin envelope, subcutaneous layer, and/or investing fascia
- The patient must be 18 years of age or older; and
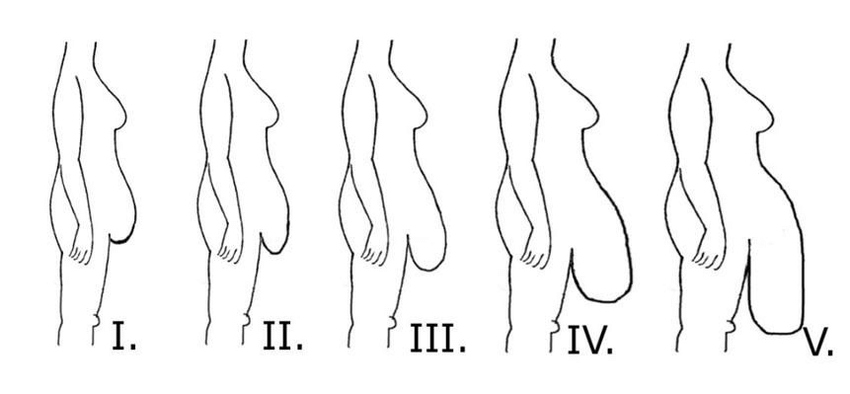
- There is photographic documentation (with member standing) of at least a Grade 2 panniculus (see Attachment) that hangs to or below the level of the pubis; and
- Surgery will correct functional impairment caused by excessive skin and subcutaneous tissue redundancy.
There is photographic documentation of any of the following chronic or recurring conditions related to excess tissue and skin folds:
o Intertrigo (bacterial or fungal infections).
o Cellulitis.
o Folliculitis.
o Panniculitis.
o Skin ulceration.
o Skin or subcutaneous abscesses.
o Monilial infection or fungal dermatitis.
o Skin necrosis
- Documentation of failure of at least three months of conservative non-surgical management by a physician other than the operating physician, such as:
o Intravenous (IV) antibiotic treatments
o Oral antibiotic treatments
o Good hygiene practices (e.g., bathing and washing daily, keeping skin dry and clean, wearing clean clothing).
o Wound care (occurring under or around the panniculus) including topical antifungals and topical and/or systemic corticosteroids
o Surgical drainage
The patient must have adequate nutrition; and
- There must be MWL demonstrated by one of the following:
o If massive weight loss occurs as a result of bariatric surgery, the procedure should not be performed for at least 18 months after the bariatric surgery and maintain a stable weight for a minimum of six (6) months, totaling 24 months or two (2) years.
o If massive weight loss occurs naturally, the patient must maintain stable weight for a minimum of 6 months after weight loss.
Panniculectomy after massive weight loss is clinically proven and, therefore, medically necessary when all of the above criteria are met.
Abdominoplasty is clinically proven and, therefore, medically necessary when performed in conjunction with a panniculectomy that meets the above criteria. In this case abdominoplasty is considered part of the panniculectomy procedure and is not separately reimbursable.
LIMITATIONS
All other indications for abdominoplasty and panniculectomy after massive weight loss are considered not medically necessary, including, but not limited to:
- There is no history of MWL through natural occurrence or bariatric surgery.
- Improving cosmesis in the absence of a functional impairment.
- Relieving neck or back pain, as there is no evidence that reduction of redundant skin and tissue results in less spinal stress or improved posture or alignment. The patient’s neck and/or back school be treated with appropriate physical therapy modalities.
- Repairing a diastasis recti.
- Minimizing the risk of hernia formation or recurrence.
- Treatment of psychological or psychosocial symptoms or complaints.
Endoscopic abdominoplasty or mini abdominoplasty is not medically necessary for any reason.
Panniculectomy when performed in conjunction with a primary abdominal surgical procedure will be considered as part of the primary surgery (e.g., incisional hernia repair) and not separately reimbursable.
- Note: All requests for panniculectomy in conjunction with repair of an incisional, umbilical, epigastric, or ventral hernia must be documented by the patient’s medical record and computed tomography scan recording the diameter of the fascial defect.
Panniculectomy is not covered when performed in conjunction with:
- Abdominal or gynecologic procedures (e.g., C-section, hysterectomy, and obesity surgery).
- Repair of abdominal wall laxity or diastasis recti to improve appearance
- Only improving activities of daily living without skin condition criteria for a panniculectomy.
- Redundancies resulting from weight loss or weight loss surgery when that tissue is without evidence of chronic infection or inflammation that is refractory to conservative treatment as outlined in the indications listed above
- Improving appearance
- Liposuction used for body contouring, weight reduction or the harvest of fat tissue for transfer to another body region for alteration of appearance of self-image or physical appearance
- All other indications unless covered in the section above
Alternative covered services:
- Analgesics
- Antibiotics
- Cortisone ointments
- Drying agents
- Topically applied skin barriers and supportive garments
Summary of Literature
The American Society of Plastic Surgeons (ASPS) Practice Parameter for Surgical Treatment of Skin Redundancy for Obese and Massive Weight Loss Patients (2007b) recommends that body contouring surgery, including panniculectomy, be performed only after an individual maintains a stable weight for 2 to 6 months. For individuals who are post-bariatric surgery, this is reported to occur 12-18 months after surgery when the BMI has reached the 25 kg/m2 to 30 kg/m2 range (Rubin, 2004). If performed prematurely, a potential exists for a second panniculus to develop once additional weight loss has occurred and the risks of postoperative complications are increased. Weight loss and BMI are important when considering panniculectomy and a significant amount of weight loss may not bring the BMI of an individual to less than 30 kg/m2; however, a panniculectomy may still be necessary (Arthurs, 2007). The American Society for Metabolic and Bariatric Surgery Consensus statement states weight loss can vary from about 25% to 70% of an individual’s excess body weight depending on the type of bariatric surgery that is performed (Buchwald, 2005).
Panniculectomy alone or with other abdominal surgical procedures, such as incisional or ventral hernia repair, or hysterectomy, is not clinically appropriate or an effective treatment of obesity. Recent meta-analyses have published mixed results of co-surgical procedures, but the studies lack documentation of a medical indication for removal of the pannus (Prodromidou, 2020; Sosin, 2020). Although it has been suggested that the presence of a large overhanging panniculus may interfere with the surgery or compromise post-operative recovery, the presence of a pannus alone is not a medical condition which warrants surgical intervention. Removal of a pannus, for reasons other than those in the criteria for medical necessity is therefore considered cosmetic and not medically necessary.
The literature addressing abdominoplasty and surgical repair of diastasis recti confirms the cosmetic benefits of these procedures. However, improvements in physical functioning, cessation of back pain, and other positive health outcomes have not been demonstrated. Carloni and colleagues conducted a systematic-review (2016) and confirmed that the quality of evidence surrounding abdominoplasty remains low and no standardization of surgical approaches has been established. Winocour (2015) reported results of a study which included 25,478 abdominoplasties and found high complication rates, compared to other cosmetic procedures, especially when abdominoplasty was combined with other procedures. Massenburg (2015) reported outcomes from 2946 abdominoplasties and found 8.5% of subjects were readmitted due to complications and 5% required revision surgery. At this time, the evidence does not support abdominoplasty when done to remove excess abdominal skin or fat, with or without tightening lax anterior abdominal wall muscles, as an effective treatment for any medical condition, though it is an effective cosmetic procedure (ASPS Practice Parameter, 2007b).
Panniculus Severity Grading Scale
- Grade I patients with a panniculus that covers the hairline and the mons pubis but not the genitals.
- Grade II extends to cover the genitals.
- Grade III extends to cover the upper thigh.
- Grade IV extends to cover the mid‐thigh.
- Grade V extends to cover the knees or beyond.
References
Centers for Medicare and Medicaid Services. 2021. Cosmetic and Reconstructive Surgery. Retrieved from https://www.cms.gov/medicare-coverage-database/view/lcd.aspx?lcdid=35090&ver=78&=
American Society of Plastic and Reconstructive Surgeons (ASPS). Practice parameter for surgical treatment of skin redundancy for obese and massive weight loss patients. 2007b. Available at: http://www.plasticsurgery.org/Documents/medical-professionals/health-policy/evidence-practice/Surgical-Treatment-of-Skin-Redundancy-Following-Massive-Weight-Loss.pdf. Accessed on December 28, 2020
Arthurs ZM, Cuadrado D, Sohn V, et al. Post-bariatric panniculectomy: pre-panniculectomy body mass index impacts the complication profile. Am J Surg. 2007; 193(5):567-570
Buchwald H; Consensus Conference Panel. Consensus conference statement bariatric surgery for morbid obesity: health implications for patients, health professionals, and third-party payers. Surg Obes Relat Dis. 2005; 1(3):371-381.
Carloni R, De Runz, Chaput B et al. Circumferential contouring of the lower trunk: indications, operative techniques, and outcomes-a systematic review. Aesthetic Plast Surg. 2016; 40(5):652-668.
Massenburg BB, Sanati-Mehrizy P, Jablonka EM, Taub PJ. Risk factors for readmission and adverse outcomes in abdominoplasty. Plast Reconstr Surg. 2015; 136(5):968-977.
Prodromidou A, Iavazzo C, Psomiadou V, et al. Safety and efficacy of synchronous panniculectomy and endometrial cancer surgery in obese patients: a systematic review of the literature and meta-analysis of postoperative complications. J Turk Ger Gynecol Assoc. 2020 Jan 13
Rubin JP, Nguyen V, Schwentker A. Perioperative management of the post-gastric-bypass patient presenting for body contour surgery. Clin Plast Surg. 2004; 31(4):601-610.
Sosin M, Termanini KM, Black CK, et al. Simultaneous ventral hernia repair and panniculectomy: A systematic review and meta-analysis of outcomes. Plast Reconstr Surg. 2020; 145(4):1059-1067
United States Food and Drug Administration.(2020). Computed Tomography. https://www.fda.gov/radiation-emitting-products/medical-x-ray-imaging/what-computed-tomography
Winocour J, Gupta V, Ramirez JR, et al. Abdominoplasty: risk factors, complication rates, and safety of combined procedures. Plast Reconstr Surg. 2015; 136(5):597e-606e.
Ito, E., Kitajima, M., Tsutsui, N. Stomaplasty with panniculectomy in an obese patient with stomal retraction: A case report. International Journal of Surgery Case Reports May 2016; S2210-2612(16)301572. Accessed on 12/20/2016.
Janniger, K.C., Schwartz, R.A., Szepietowski, J.C., Reich, A. Intertrigo and Common Secondary Skin Infections. American Family Physician 2005; 1; 72 (5):833-838. Accessed on 12/16/2016.
Ponce J. New procedure estimates for bariatric surgery: what the numbers reveal. Connect. May 2014.
American Society for Metabolic and Bariatric Surgery 2014. Accessed on 12/19/2016.
Panniculectomy for Abdominal Contouring Following Massive Weight Loss. September, 2012. Hayes: Transforming Healthcare with Evidence. Accessed on 12/6/2016.
Rao, R.S., Gentileschi, P., Kini, S.U. Management of ventral hernias in bariatric surgery. Surgery for Obesity and Related Diseases 2011; 110-116. Accessed on 12/6/2016.
Erdmann, D. Resection of Panniculus Morbidus: A Salvage Procedure with a Steep Learning Curve. Plastic & Reconstructive Surgery 2008; 122(4):1290. Accessed on 12/19/2016.
American Society of Plastic Surgeons (ASPS). Practice Parameter for Surgical Treatment of Skin Redundancy Following Massive Weight Loss. January, 2007. Accessed on 12/6/2016.
American Society of Plastic Surgeons (ASPS). ASPS Recommended Insurance Coverage Criteria for Third Party Payers: Abdominoplasty and Panniculectomy Unrelated to obesity or Massive Weight Loss 2007. Accessed on 12/19/2016.
Constantine, R.S., Davis, K.E., Kenkel, J.M.: The Effect of Massive Weight Loss Status Amount of Weight Loss, and Method of Weight Loss on Body Contouring Outcomes. Aesthetic Surgery Journal 2014; 34(4). Accessed on 12/19/2016.
Gurunluoglu R. Panniculectomy and redundant skin surgery in massive weight loss patients: current guidelines and recommendations for medical necessity determination. Ann Plastic Surgery 2008; 61(6):654-657. Accessed on 12/20/2016.
Harth, K.C., Blatnik, J.A., Rosen, M.J. Optimum repair for massive ventral hernias in the morbidly obese patient—is panniculectomy helpful? American journal of surgery 2007; 201(3):396-400. Accessed on 12/20/2016.